Wow, great experience having my wisdom teeth removed which I never thought I’d ever say. Clinic was very organized, all the staff I dealt with was very friendly and helpful, and the extraction and aftercare was excellent. I’d get my teeth removed there again if I could! Very happy!
General Information

TMJ disorders develop for many reasons. You might clench/grind your teeth, tighten your jaw muscles and stress your TM joint. You may have a damaged jaw joint due to injury or disease. Whatever the cause, the results may include a misaligned bite, pain, clicking, grating noises when you open your mouth or trouble opening your mouth widely.
Often no one treatment can resolve TMJ disorders completely and the treatment takes time to become effective. If you have been referred to an oral surgeon for your TMJ, most likely less invasive treatment options have not provided you the relief you are striving for. An oral surgeon can provide you with the following treatment options:
- Botox injections of facial muscles
- Temporomandibular joint arthrocenthesis
- Temporomandibular joint surgery
Botox of Facial Muscles
Procedure
Botox is used in TMJ (temporomandibular joint) disorders and associated muscle tension and pain. These injections may be used alone or in conjunction with surgical treatments. A consultation with one of our doctors will determine if you may are a candidate for this treatment.
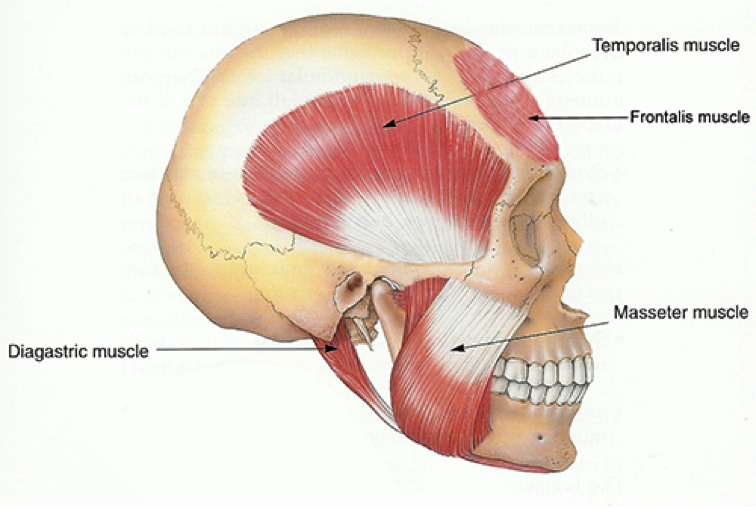
Located on both sides of the head at the point where the jawbone meets the skull, the temporo-mandibular joint (TMJ) is used during talking, eating, swallowing, and other everyday activities. If the muscles of the jaw are overworked through excessive teeth grinding, a person may suffer sharp pain in the muscles of the jaw. The Botox can relieve muscles tension and pain by making the muscles unable to engage in the powerful, often unconscious movement of the jaw that produces the clenching and the pain. Many patients have found relief from their symptoms with these injections.
This procedure is done in office and takes approximately 10- 30 minutes depending on how many sites and how much Botox will be used.
Recovery
Minimal to mild discomfort may be felt during the injections but generally no pain medication is required. There may be mild temporary bruising, numbness, or redness around the injection sites. If experiencing some discomfort or stiffness often an over the counter medication such as Ibuprofen (Advil) or Acetaminophen (Tylenol) can be helpful. Generally it can take a few days to a week before the positive effects of the injections can be felt.
Most patients can return to normal activities almost immediately. To avoid spreading the toxin to other muscles, patients should not rub or massage the areas injected with Botox and remain upright for a few hours.
Risks
As with any medical procedure there are possible risks and side effects when using Botox for TMJ treatment. Since this is a non-surgical treatment procedure, the risks and possible complications are infrequent, minimal and temporary.
The most common reported side-effects of Botox treatment are pain, redness or bruising at spot of injection, and muscle weakness. Less common side effects include temporary eye-lid droop.
Another limitation to Botox injection for TMJ treatments is that there is a possibility of developing antibodies that would render the TMJ treatments less and less effective over time. This resistance could be delayed by using the lowest effective dose possible over the longest intervals of time. Botox injection treatments should be avoided during pregnancy and lactation.
Temporomandibular Joint (TMJ) Arthrocentesis
Procedure
An oral and maxillofacial surgeon will often recommend TMJ arthrocentesis when conservative therapies have not proven to be successful. This simple procedure is used to provide relief from temporomandibular joint pain and discomfort. The purpose of this procedure is to remove tissue breakdown products and reduce inflammation that may have accumulated in the affected joint. Although pain relief is never guaranteed, many patients have found this procedure to be effective in managing their symptoms.
The patient is placed under a general anaesthetic. Once asleep, the surgeon inserts a sterile needle into the temporomandibular joint space. A syringe is attached to the needle and used to push sterile fluid into the joint space. A second needle is then inserted so that the joint can be washed out. Fluid enters the joint through one needle and leaves out the other. This removes the inflamed fluid from the joint. Some surgeons will also use a steroid (anti-inflammatory medication) at the end of the procedure. It is injected and left in the joint prior to needle removals.
Recovery
See The Arthrocentesis Post-Operative Care.
Open Joint Surgery
There are many types of open joint surgeries. The surgeon makes a cut in a skin crease just in front of the ear. This exposes the jaw joint. The surgeon may repair, reposition, or replace the disc with your own tissue or an artificial disc. Scar tissue or bony growths in the jaw joint can also be removed. Open-joint arthroplasty is done under general anesthesia. You can normally expect to go home the same day.
Your Oral Surgeon May Suggest This Type Of Surgery If:
- Your TMJ is degenerating
- There are tumors in or around your TMJ
- The joint is severely scarred or contains chips of bone
- Arthrocentesis is not possible or has not succeeded in the past.
- The joint is fused together by bony growth (ankylosis).
Your surgeon at your consult will further discuss the procedures, risks, benefits and recovery phase with you.